Approximately one in eight couples struggle with infertility in the United States. That’s over 6.5 million people annually who have trouble conceiving. Apart from the obvious reproductive challenges, infertility can take a tremendous mental toll.
However, infertility does not mean one cannot conceive. While the road to recovery will not be without its challenges, modern treatment protocols combined with guidance from a seasoned fertility expert may significantly boost your chances of becoming a parent.
Dr. Michael Allon, a board-certified infertility specialist at the Advanced Fertility Center of Texas, has been at the forefront of reproductive healthcare for over 20 years. Dr. Allon’s extensive experience working with infertile couples makes him ideal to guide you through to a successful and stress-free journey to parenthood.
Let’s take a closer look at what might cause female infertility and how Pelvic Laparoscopy can help you manage it along with improving the odds of pregnancy.
What Is Female Pelvic Laparoscopy?
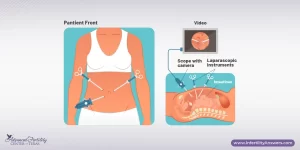
Laparoscopy is a surgical process used in reproductive medicine in order to diagnose or treat infertility issues. The procedure uses an instrument called a laparoscope, which is a thin device with an attached camera. It allows the surgeon to easily assess any organ damage and disease within the pelvic region. Unlike other major surgeries, a pelvic laparoscopy only requires small incisions, each about half an inch. It’s minimally invasive and promotes rapid recovery.
From PCOS and obesity to endometriosis, several conditions may make it challenging for you to conceive. Laparoscopy is often recommended to diagnose and treat the following issues.
-
Endometriosis
Endometriosis is a painful disorder characterized by the growth of additional tissue outside of the uterus. The surrounding areas can then become inflamed or swollen, which explains the pain, lesions, and scar tissue. Laparoscopic surgery can effectively treat mild to severe cases of endometriosis. The surgeon will make two small incisions; one to insert the viewing instrument (laparoscope) close to your navel and the other one to remove the endometrial tissue.
-
Polycystic Ovary Syndrome (PCOS)
PCOS is another condition that can affect a woman’s fertility. It is characterized by a hormonal imbalance where the male hormones produced are higher than normal. This imbalance can increase the risk of infertility, diabetes, and obesity among others. Some of its symptoms are hair loss, acne, and depression.
Your doctor may advise laparoscopic ovarian drilling. It involves making three to eight tiny punctures into the ovaries. This may restore ovulation in PCOS patients who have not responded well to fertility medication.
-
Fibroid Tumors & Fallopian Tube Blockage
Fibroids are non-malignant muscle tissue that can develop in and around the uterus. You may not be aware that you have it because most women do not exhibit symptoms. Gametes are reproductive cells that both men and women have. These cells must combine for a pregnancy to happen. Fibroid growth causes a blockage in the fallopian tubes which prevents male and female gametes from merging thereby causing infertility. A laparoscopic procedure may be able to unblock or repair a damaged fallopian tube.
-
Pelvic Adhesions
This is a condition when scar tissues form between female pelvic organs such as the uterus, ovaries, fallopian tubes, and bladder. The condition can compromise your ability to conceive by disrupting normal ovarian and uterus function by banding them with other surfaces. The adhesions prevent the sperm from reaching the egg, therefore, preventing pregnancy. Plus, they can be quite thick and make sexual intercourse quite painful.
-
Unexplained Infertility
An unexplained infertility diagnosis is the last thing you’d want to hear from your doctor. It’s a frustrating diagnosis because the cause of your infertility cannot be precisely determined. As controversial as this diagnosis is, it doesn’t necessarily mean that you are out of options.
Though it is termed “unexplained,” there are several possible explanations for what’s causing infertility. It can be an undiagnosed underlying condition, mild endometriosis, and poor egg and sperm quality, among others. Pelvic laparoscopy is usually recommended not just to diagnose but to treat the condition altogether.
Advantages of Pelvic Laparoscopy Over Open Surgery
As compared to open surgery, laparoscopy offers a host of benefits. Let’s explore further:
- To begin with, only small incisions are made in the pelvic & abdominal areas. This makes it a minimally invasive and quick surgical procedure.
- Laparoscopy offers an equally effective treatment path for patients who are not inclined towards conventional open surgery. The pain is significantly lower and the recovery period is shorter in most cases. The usual recovery period for open surgery could be anywhere between 4-8 weeks. With laparoscopy, recovery takes no more than 2-3 weeks.
- As compared to a hospital stay of over 1 week for usual surgery, you could be back home within 2 nights. The reduced hospice stay will also translate into a sizeable medical bill savings
- With laparoscopy, doctors can pinpoint and understand any causes of infertility and other issues with a much higher degree of accuracy thus improving the odds of pregnancy.
- The small incisions also mean that you won’t have to deal with prominent tissue scars.
- There is a reduced rate of infection since the procedure doesn’t require extended handling of internal organs.
When is a Female Pelvic Laparoscopy Necessary?
Your doctor may recommend a pelvic laparoscopy if you have unexplained infertility, a suspected diagnosis, or a known condition. However, it’s not a given that those struggling with infertility should have a laparoscopy.
Laparoscopy is typically a last resort after you have exhausted other infertility diagnostic options. But if your infertility struggles are accompanied by pelvic pain, your doctor will likely recommend the procedure. This can include pain from sexual intercourse, severe menstrual cramps, or pain from potential endometriosis, pelvic inflammatory disease, or an ectopic pregnancy.
What To Expect From Laparoscopy Surgery
The following section discusses how the surgery is conducted, risk factors, and how to address any concerns or queries you may have.
Procedural Overview
- The female pelvic laparoscopy procedure typically requires general anesthesia, although in some cases local anesthesia is appropriate.
- The surgeon inserts the laparoscope into the abdomen through the small, half-inch small incision. S/he may also examine the reproductive organs with other surgical instruments if necessary. This can include a uterine manipulator, which allows for movement of the vagina, cervix, and uterus, exposing other views of the pelvic anatomy.
- The doctor may also take tissue samples. If they do note a problem, the surgeon may immediately treat the condition — they may remove scar tissue, or repair or remove parts of the ovaries, uterus, or uterine tubes. Once complete, the surgeon removes the instruments, stitches up the incisions, and bandages the area.
- You will likely have a sore throat after you wake up. That’s because a tube is placed down your throat to facilitate normal breathing during surgery. This tube will be taken out before you wake up.
- You can expect to feel tired from the anesthesia, but this should dissipate throughout the day. You will likely feel some discomfort and bloating in the abdomen, along with some shoulder or back pain.
Recovery
Most people can be driven home on the same day and resume normal activities within a day or two. You should avoid lifting anything over ten pounds or exercising for at least two weeks. The benefit of laparoscopy is that it avoids many of the problems of an open surgery — there is lower pain, a faster recovery, and a reduced risk of infection.
Pre and Post-Surgical Communication
Please consider that laparoscopy is still a surgery, and your surgeon will inform you of any associated risks before the procedure. It is also worth noting that AFCT follows up with its patients 2 weeks after the procedure to ensure that everything’s okay and that there are no side effects to worry about.
Possible Risk Factors
Like most surgical procedures, laparoscopy has certain risks. However, modern technology and surgical protocol make it very safe, and the American Society of Reproductive Medicine reports that only 1 to 2 percent of the patients develop minor complications.
Some common complications include:
- Bladder infection after surgery
- Skin irritation around the areas of the incision
Other less common risks include:
- Formation of adhesions
- Hematomas of the abdominal wall
- Infection
Although highly unlikely, some serious complications include:
- Damage to the organs or blood vessels found in the abdomen (further surgery may be needed to repair any damage caused.)
- Allergic reaction
- Nerve damage
- Urinary retention
- Blood clots
- Anesthesia complications
- Mortality (around 3 in every 100,000)
Contact Us with Your Laparoscopy Questions
It doesn’t matter what’s preventing you from getting pregnant, we at the Advanced Fertility Center of Texas, intend to provide you with the knowledge to help you conceive successfully.
If you have questions about an upcoming female pelvic laparoscopy or are curious if the procedure could help you diagnose your reproductive condition, we invite you to get in touch with the Advanced Fertility Center of Texas. Please call us at (713) 467-4488 and our team will gladly guide you through.