Symptoms of PCOS
Lack of ovulation or less than eight cycles per year, elevation of testosterone levels in the blood, clinical evidence of male pattern hair growth or acne, and polycystic ovaries (enlarged ovaries with 12 or more small follicles).
What is PCOS?
PCOS is difficult to diagnose because no test or combination of tests offer a definitive diagnosis. However, PCOS patients usually have elevated androgens (male hormones) and cysts can often be observed on the ovaries. There is a strong association between PCOS and insulin resistance with at least 80% of women with PCOS being insulin resistant.
Different patients experience different manifestation of the syndrome, which complicates both diagnosis and treatment.
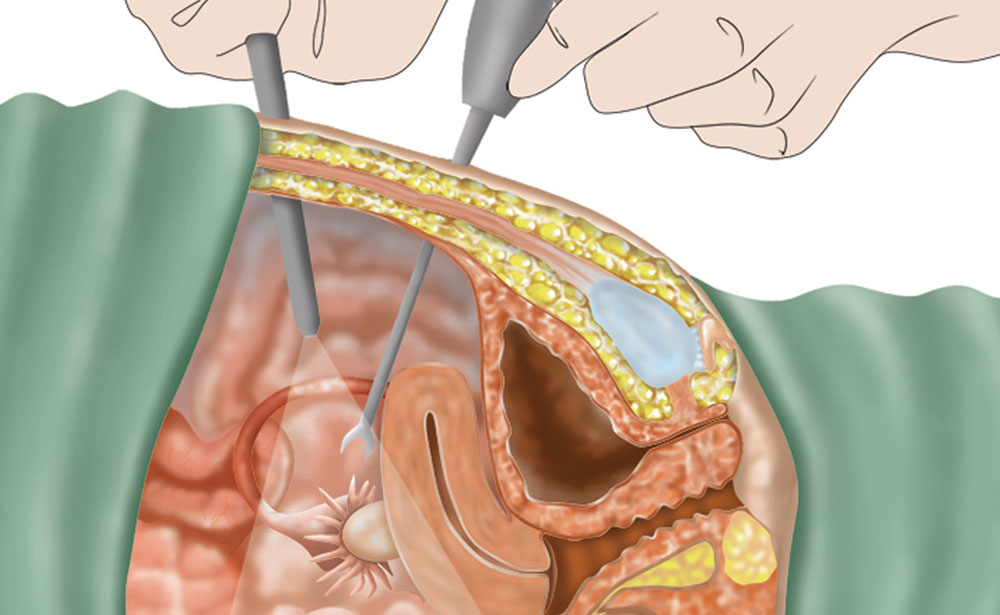
Women with PCOS usually present with enlarged ovaries with numerous enlarged peripheral cystic follicles and increased central stroma (the middle section of the ovary, which produces androgens). Many studies suggest that the polycystic appearance is due to increased production of androgens, which leads to lack of ovulation resulting in the follicle atresia (arrest of development).
“Syndrome X” is a new term, which denotes a combination of insulin resistance or diabetes, dyslipidemia, hypertension, and central obesity. While insulin resistance and type II diabetes are frequently associated with obesity, there are women of normal weight who are afflicted as well. Syndrome X may be associated with PCOS.
In 1990, the National Institute of Health established the following criteria for Polycystic Ovary Syndrome (PCOS) diagnosis:
· Elevated Testosterone (Hyperandrogenism and/or Hyperandrogenemia)
· Lack of Ovulation (Oligoovulation)
· Exclusion of Other Known Disorders
In 2003, PCOS was defined
as having at least two of the
following three conditions:
· Lack of Ovulation or Less than Eight Cycles Per Year
· Elevation of Testosterone Levels In the Blood or Clinical Evidence of Increased Male Hormones
· Polycystic Ovaries (Enlarged Ovaries With 12 or More Small Follicles)